Your care provider, whether one of the doctors here at Migraine Relief Center or another medical professional, will begin by explaining the simplest and least invasive treatment options that are appropriate for your migraines. If medication or other treatments are effective, you may be able to go back to your daily life with your pain well controlled. However, if less-invasive options don’t provide the relief you need, migraine surgery may be an option to consider discussing with your Physician.
For migraine patients who don’t respond well to other treatments, surgery may be a migraine treatment that restores their quality of life. The goal of migraine surgery is headache and migraine reduction. After surgery, patients may still get headaches, but could experience a decrease in headache frequency, duration, and/or pain severity.
Here is helpful information about migraine surgery that you can discuss with your Doctor.
Migraines have long been associated with the compression and irritation of key nerves in your face and head. These triggers may be chronic, may have genetic causes—just the way your personal anatomy is put together, or may be the result of changes that take place over time. Surgically relieving the pressure on compressed nerves may reduce the frequency, severity and duration of headaches, or even eliminate them altogether.
Physicians noticed a connection between anatomy and headaches back in 1919. By the 1980s, patients were reporting relief from headaches after sinus surgery reduced contact between nerves and nasal turbinates or septum. ENT specialists performing the surgeries began to theorize that pressure created by such contact may be a trigger for headache pain.
In the early 2000s, plastic surgeon Bahman Guyuron, M.D., observed that patients who suffered chronic migraine (at least 15 headaches per month for at least three months) frequently reported fewer headaches—or none at all—after undergoing certain cosmetic procedures such as brow lifts. He conducted research, and developed the theory that migraine pain is caused by inflamed trigeminal nerve branches in the head and neck. These nerves become irritated when surrounding tissues, such as muscles and fascia, apply excessive pressure. Dr. Guyuron believed that if a patient’s specific trigger sites could be pinpointed, surgical intervention might stop the irritation, which could reduce inflammation and possibly eliminate the migraine trigger.
Today there have been multiple articles published studying migraine surgery.
There are four sites generally considered to be likely trigger points. Each has a specific surgical procedure to treat the pressure and irritation.
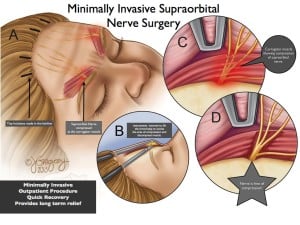
Frontal headaches (starting above the eyebrows) may be caused by irritation of the supratrochlear and suborbital nerves in the glabellar area. The surgeon endoscopically resects the corrugator and depressor supercilii muscles through a tiny incision.
Rhinogenic or nasal headaches (behind the eyes), may be treated with a septoplasty (see Types of Migraine Surgery below).
Occipital headaches (originating in the back of the neck) may be caused when the greater occipital nerve is impinged by the semispinalis capitis muscle. During surgery the muscle is resected and the nerve shielded from further irritation.
Migraine surgery may reduce the irritation and compression of trigger nerves, either by correcting the tissue surrounding the nerves or by blocking the pain signals.
There are different surgical treatments for migraine: nerve release and pain blocking.
The tissue surrounding a nerve—the muscle, fat, or other structures—can impinge or compress the nerve and trigger migraine pain. Since a number of different nerves can be triggers, there are several different types of corrective surgeries. The surgery that may work for you depends on many factors such as the location of your personal triggers and pain.
 layer known as fascia are usually the cause. The procedure we perform, we have adapted the acronym, M.I.G.O.N.E., or Minimally Invasive Greater Occipital Nerve Entrapment. The greater occipital nerve provides sensation for much of the back and top of the head (and can cause pain as far forward as the eyes). It’s also a common site for migraine triggers. The surgeon removes enough of the tissue surrounding this large nerve to free it and allow it to function normally. This procedure takes about 2-3 hours to perform.
layer known as fascia are usually the cause. The procedure we perform, we have adapted the acronym, M.I.G.O.N.E., or Minimally Invasive Greater Occipital Nerve Entrapment. The greater occipital nerve provides sensation for much of the back and top of the head (and can cause pain as far forward as the eyes). It’s also a common site for migraine triggers. The surgeon removes enough of the tissue surrounding this large nerve to free it and allow it to function normally. This procedure takes about 2-3 hours to perform.Both M.I.S.O.N. and M.I.G.O.N.E. surgeries are minimally invasive, performed using HD cameras, and are generally performed as outpatient procedures.
Please note, there are no guaranteed results for migraine surgery and results may vary. In a study published in Plastic and Reconstructive Surgery, 88% of the patients surveyed five years after their migraine surgery reported at least 50% reduction in the frequency, severity and duration of their headaches. The University of Wisconsin–Madison reports studies showing success rates greater than 70%, with about a third of those patients reporting their headaches eliminated completely. A UT Southwestern Physician claims an amazing 60% of his patients report being pain free after surgery, and almost 90% report at least a 50% reduction in pain.
Your migraine surgical procedure may be covered by your insurance. Just as BOTOX® treatments for migraine are now often covered, insurance providers have begun to recognize that surgical intervention is much less costly over the long run. Check with your insurance provider.
There are no guarantees for any medical treatment, and every individual case is different, but the surgical treatment MRC offers, aims to reduce the number and severity of your migraines. While we can’t guarantee specific results, 90% of our patients say their migraines are less frequent and/or don’t last as long, while 50% say they’re migraine-free within months of their surgery.
There are a number of factors to consider in deciding if migraine surgery is your best option.
Your history
Our surgeons will need as much information about all your medical conditions as possible. We’ll need
Consultation
Our surgeons will talk to you about your migraines, and your medical history. We’ll examine you to determine if nerve compression could be causing your headaches, or if there are other indications that you have which may respond to surgical treatment.
Test results
There are treatments that give a similar “temporary version” of the outcome that surgery might provide, such as BOTOX® or nerve blocks. If you haven’t had such treatment in the past, our surgeons will administer them, to evaluate how much help surgery might be in your case.
Migraine Diary
After your diagnostic treatment, you’ll need to keep a written record of your symptoms for several weeks. Reviewing this pain diary can reveal how beneficial surgery might be for you.
Successful migraine surgery requires an expert plastic or peripheral nerve surgeon to correctly identify and locate your trigger sites. MRC’s Khorsandi brothers are board-certified and hold many top honors in their respective fields. Their specialized training and years of experience make them experts in evaluating a patient’s trigger sites and determining how much relief surgery can provide.
Our pre-surgical selection process includes diagnostic and therapeutic testing to provide you with the best possible results. You’ll have a physical exam, give a thorough medical history, and be asked to keep a Migraine Diary. If you’re considered a candidate for surgery, you’ll most likely receive botulinum toxin (BOTOX®), nerve blocks, or steroid substitutes to evaluate your response to soothing the nerves at your trigger point. That’s an important step in predicting your surgical outcome. Please note, BOTOX® is not always prognostic of how the surgery will do, but nerve blocks are. Patients that have had failure with BOTOX® are still considered good candidates for surgery, as long as there is some response to the nerve block procedure.
Through every step, we make sure your potential benefits outweigh the risks of surgery, and that you know what to expect.
As with any medical procedure, no one can guarantee results. However, our exacting pre-surgical protocol is designed to make sure your treatment gives you the best possible outcome.
While MRC’s surgical procedures are minimally-invasive, every surgery involves risk. You may experience side-effects, and complications are possible. If you have any questions or concerns, please be sure to discuss them with your physician.